Authors: Robert Goodnough, MD (EM Resident Physician, UCSF-ZSFG Emergency Medicine Residency Program), Karla Canseco, MD (EM Resident Physician, UCSF-ZSFG Emergency Medicine Program), and Marianne Juarez, MD (Assistant Clinical Professor of Emergency Medicine, UCSF-ZSFG Medical Center) // Edited by: Jennifer Robertson, MD, MSEd and Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UTSW / Parkland Memorial Hospital)
Case:
A 65 year-old presents to the emergency department (ED) via emergency medical services (EMS) due to respiratory distress that awakened him from sleep. EMS reports that, upon their arrival, the patient had an oxygen saturation of 85% on room air. Continuous positive airway pressure (CPAP) was provided to the patient and his oxygen saturation improved to 94%. The CPAP also improved the patient’s work of breathing.
On examination in the ED, the patient is tachypneic. He also demonstrates rales, supraclavicular retractions, and is in atrial fibrillation with heart rate (HR) in the 110s. His blood pressure (BP) is 205/104 mmHg. A nitroglycerin drip is ordered and respiratory therapy is called to place the patient on bi-level positive airway pressure (BiPAP). At this point, one of your seasoned colleagues mentions that he remembered a time when all heart failure patients were intubated.
You tuck your endotracheal (ET) tube into your back pocket and you wonder if your patient will eventually need this…
Introduction:
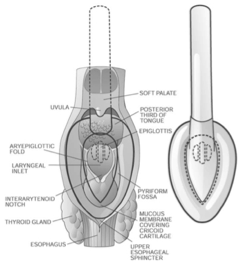
Noninvasive Positive Pressure Ventilation (NIPPV) is mechanical ventilation that is provided via nasal prongs, a full or oral-nasal facemask, or mouthpiece. Different modes of mechanical ventilation are available, but the most commonly used methods are CPAP and BiPAP1. The majority of evidence in NIPPV does not differentiate between CPAP and bi-level, or other modes of NIPPV, and the majority of outcomes and data are applied to NIPPV as a generalized intervention.
![PIC1]()
(photo courtesy of Kai Romero, MD)
Why avoid endotracheal intubation?
Endotracheal intubation is a life-saving intervention when applied skillfully, but its attendant risks are well described. Staving off intubation has been shown to decrease complications such as hypotension, arrhythmias, death, and nosocomial infections. Intubation also places patients at an increased need for sedation and invasive procedures2. Noninvasive ventilation has become commonplace in the ED to treat respiratory failure and prevent intubation1.
Some Definitions:
- CPAP: applies constant pressure throughout the breathing cycle to increase functional residual capacity (FRC) by recruiting alveoli, decreasing work of breathing, and improving oxygenation. It is best given in hypoxemic patients 1,3.
- PEEP/EPAP: Positive End Expiratory Pressure, which is the alveolar pressure before inspiratory flow begins. Adding PEEP helps decrease the amount of work required to initiate a breath. It also helps to decrease atelectasis1,4.
- Bi-level: Cycled ventilation between Inspiratory Positive Airway Pressure (IPAP) and Expiratory Positive Airway Pressure/PEEP1. BiPAP supports ventilation and increases oxygenation.
- Pressure Support: The difference between EPAP and IPAP is referred to as pressure support. Pressure support makes it easier to draw larger tidal volumes1,4.
Applications for NPPV/Bi-level
1. Chronic Obstructive Pulmonary Disease (COPD)
In COPD, acute respiratory failure manifests as hypoxic, hypercapneic respiratory failure with collapse of small airways. Hyperinflation also occurs. Acute respiratory failure from COPD leads to increased work of breathing, acidosis, altered mental status, and ultimately coma, decompensation, and death5
Bi-level ventilation is a primary treatment option in COPD with good evidence for success5. When compared to usual medical care, bi-level ventilation decreases the risk of death (relative risk reduction 48%) and intubation rates (RRR 60%)5.
Number Needed to Treat (NNT) for mortality benefit = 10
NNT to prevent intubation = 4
Furthermore, when comparing patients with moderate and severe acidosis, bi-level ventilation decreased mortality, rates of intubation, and lengths of stay. It also improved work of breathing, acidosis, and PaC02 levels. Finally, regarding these outcomes, there were no significant differences between more and less acidotic patients at admission5,6.
Indications for NIPPV/bi-level ventilation6
1. pH <7.35or PaC02 >45 mmHg
2. Severe dyspnea with signs of increased work of breathing
3. Caution: In severe respiratory acidosis (pH <7.25), failure rates of NIPPV may be as high as 50%1
Common Initial Settings:
- IPAP 8-20 cm H2O (up to 30 cm H20)
- EPAP 2-6 cm H2O to overcome intrinsic airway collapse3,5,7
- Begin with either high IPAP and then titrate down, or low and titrate high. Both are reasonable, but require close monitoring to meet ventilation goals.7 Each patient is different.
- Endpoints for physiologic improvement: at 1 hour, reassessment should be made. Decisions regarding treatment failure, worsening clinical status of bi-level should be made early.5
2. Cardiogenic Pulmonary Edema (CPO)
Acute cardiogenic pulmonary edema is a common and potentially fatal cause of acute respiratory distress. CPO is related to a critical interaction between worsening left ventricular systolic function and an acute increase in systemic vascular resistance that results in rapid accumulation of fluid in the interstitium of the lung. This leads to decreased lung compliance, increased airway resistance, hypoxia, decreased diffusion capacity, and hypercarbia from muscle fatigue8.
Bi-level offers the advantage of improving both cardiac and pulmonary function by providing pressure support with IPAP and EPAP/PEEP. IPAP assists ventilation, which decreases the work of breathing and assures adequate ventilation. The EPAP/PEEP increases the FRC by recruiting collapsed alveoli, improving oxygenation, and helping to force interstitial fluid back into the pulmonary vasculature9,10.
Bi-level ventilation also increases intrathoracic pressure, which can lead to decreased left ventricular (LV) end diastolic volume. This results in decreased afterload and increased LV ejection fraction/stroke volume. Thus, the heart muscle is stretched less, and placed at a steeper part of the Starling curve. This results in stronger LV contractions, and reductions in BP and HR11.
![PIC2]()
(Figure: in the failing heart, NIPPV both decreases preload and also shifts the Starling curve (decreases afterload) to augment cardiac performance)12,13
Common Initial Settings:
· IPAP: 10 to 20 cm H20
· EPAP: 5 to 10 cm H20
· I:E ratio of IT to ET and is usually set at 1:3 or 1:4 (Inspiratory to Expiratory ratio)
Evidence for Bi-level ventilation in CPO:
Unfortunately, most of the evidence for NIPPV for CPO is centered on CPAP with few trials comparing the two modalities (CPAP and bi-level) head-to-head.
In a Cochrane review looking at NIPPV in CPO, CPAP alone has been proven to decrease intubation rates and to decrease in-hospital mortality, without the same benefit seen using bi-level ventilation14.
In the treatment of CPO, controversy regarding the safety of bi-level ventilation stems mainly from a single small study comparing the two NIPPV modalities. This study showed a more rapid improvement in vital signs, dyspnea and arterial blood gas (ABG) results with bi-level, but it also showed higher rates of myocardial infarction (MI) with bi-level ventilation15. However, subsequent trials comparing CPAP and bi-level showed no difference in MI rates, but decreased intubation rates for those treated with bi-level, especially in patients presenting with hypercarbia16,17.
A trend that holds true is that bi-level leads to rapid improvement in physiological parameters such as respiratory rate, pH, PaCO2, PaO2, HR, work of breathing, afterload, preload, cardiac index, and ejection fraction. However, more studies need to be performed to show a clear benefit in patient mortality and consistently decreased intubation rates18–21.
Indications for NIPPV in CPO:
1. Increased work of breathing
2. Hypercapnia and respiratory failure
3. Asthma
In asthma, NIPPV/bi-level ventilation might help to overcome intrinsic auto-PEEP, to decrease ventilation/perfusion (V/Q) mismatch by increased recruitment of alveoli, and to have a direct bronchodilatory effect in order to decrease work of breathing22.
In the mechanical ventilation of an asthmatic, one should carefully weigh the risk of critical error if the patient is not allowed a prolonged period of expiration in order to prevent “auto-PEEP”. Auto-PEEP is a condition where inhaled breaths are progressively delivered to lungs that have not returned to their FRC. This can subsequently lead to life-threatening hypotension and severe barotrauma, such as pneumothorax2.
Complications from intubation in a severe asthmatic can be severe, including cardiovascular collapse, pneumothorax, and prolonged intubation23. However, a systematic review comparing NIPPV to medical care did not find a significant benefit to mortality or decreased rates of intubation, though these end points were likely limited by small numbers of patients studied in the intervention22.
Given the risks of intubation, and the purported physiologic benefits of bi-level ventilation to a severe asthmatic, NIPPV is a reasonable treatment strategy. However, this should be done in tandem with medical management in carefully selected and monitored patients. Of note, NIPPV in asthma has not yet achieved the standard of care.
Indications for NIPPV in Asthma:
1. As a carefully applied adjunct to medical management in refractory asthma
4. Acute Respiratory failure (no pre-existing chronic lung disease)
The benefits of NIPPV is not clear in undifferentiated acute respiratory failure and the evidence is often conflicting. The use of NIPPV in undifferentiated acute respiratory failure (ARF) has shown similar mortality rates to conventional ventilation, but it has also demonstrated decreased intubation rates. On the other hand, decreased intubation rates may not apply to those with pneumonia or non-hypercapneic respiratory failure (PNA)24.
A recent multi-center trial showed no decrease in intubation rates for non-hypercapneic ARF (64% PNA) in those without chronic lung disease when compared to high flow or regular oxygen. Additionally, 90 day mortality was decreased in the high flow oxygen group compared to NIPPV. Also, delayed intubation via NIPPV did not show an association with increased mortality25.
Method of delivery and severity of illness likely affect mortality rates in patients with adult respiratory distress syndrome (ARDS) treated with NPPV, as a recent RCT showed decreased 90 day mortality in patients ventilated with helmeted NPPV compared to face mask NPPV26.
Indications:
1. There are no clearly recommended indications and it should be on a case by case basis.
5. Blunt Thoracic Trauma
In a recent meta-analysis of 219 patients with thoracic trauma, NIPPV decreased intubation rates, improved oxygenation, decreased infection rates and showed mortality rates of 3% vs 22.9% in “standard management,” which was CPAP or face mask oxygen27.
6. Special Populations:
NIPPV decreases intubation rates and in-hospital mortality when applied to acute hypoxic respiratory failure in immunocompromised patients1,28.
It may also provide a benefit to patients with palliative care needs in whom endotracheal intubation is not within their goals of care, with some studies showing reversal of acute respiratory failure and return to home1,28,29.
The use of NPPV in the ARF of decompensation of neuromuscular disease is controversial, and may not be indicated in those with rapidly progressive disease29.
Pre-oxygenation For Intubation:
Much of the focus has been on avoiding intubation, but in critically ill patients, intubation and mechanical ventilation can be life-saving; to intubate an unstable patient is perilous, with desaturation, arrhythmia, cardiovascular collapse and cardiac arrest as well recognized entities30.
Pre-oxygenation prior to intubation is the standard of care to prevent life threatening complications during intubation. Some patients display refractory hypoxia in the face of usual facemask pre-oxygenation, and failure to reach 93-95% Sp02 prior to intubation places the patient at risk for desaturation and apnea during the procedure31.
NIPPV has been shown to decrease desaturation rates in refractory hypoxia during pre-oxygenation for intubation and should be strongly considered for pre-oxygenation prior to intubation in refractory hypoxia30–32.
Pearls:
- Positive Pressure is not everything. Do not forget medical management
- Bi-level ventilation is an early “go-to” in moderate to severe COPD exacerbations
- Experienced respiratory therapists (RTs) and staff are critical to the success of non-invasive ventilation
- Once applied, reassess your patient frequently and be ready to adjust!
- Can be used to stave off intubation at the end of life
- Consider for pre-oxygenation prior to intubation
Pitfalls:
- Positive pressure can cause hypotension and decompensation if blindly applied
- Do not place a pressure mask on a damaged face or a fluid filled mouth
- Do not delay necessary intubation
- Do not let your patient Auto-PEEP
- Your severely acidotic patient is at high risk for failure: be ready to intubate.
- If your patient is not awake, then the patient should be intubated.
Who Needs It?
- Patients with moderate to severe COPD exacerbations
- Those patients with cardiogenic pulmonary edema with increased work of breathing or hypercapnia
- Patients with isolated blunt thoracic trauma
- The immunocompromised patient with hypoxic respiratory failure
- Patients who require pre-oxygenation prior to intubation
Who Does Not?
- Altered Mental Status
- Facial Trauma/Can’t Handle their own secretions
Gray Zones?
- Asthma
- Neuromuscular Disease
- Undifferentiated Hypoxic Respiratory Failure
References / Further Reading
1. Aboussouan, L. S. & Ricaurte, B. Noninvasive positive pressure ventilation: Increasing use in acute care. Cleve. Clin. J. Med. 77, 307–316 (2010).
2. Leatherman, J. Mechanical ventilation for severe asthma. Chest 147, 1671–1680 (2015).
3. Bolton, R. & Bleetman, A. Non-invasive ventilation and continuous positive pressure ventilation in emergency departments: where are we now? Emerg. Med. J. EMJ 25, 190–194 (2008).
4. Appendini, L. et al. Physiologic effects of positive end-expiratory pressure and mask pressure support during exacerbations of chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 149, 1069–1076 (1994).
5. Ram, F. S. F., Picot, J., Lightowler, J. & Wedzicha, J. A. Non-invasive positive pressure ventilation for treatment of respiratory failure due to exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. CD004104 (2004). doi:10.1002/14651858.CD004104.pub2
6. Pauwels, R. A., Buist, A. S., Calverley, P. M. A., Jenkins, C. R. & Hurd, S. S. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 163, 1256–1276 (2001).
7. Prinianakis, G., Delmastro, M., Carlucci, A., Ceriana, P. & Nava, S. Effect of varying the pressurisation rate during noninvasive pressure support ventilation. Eur. Respir. J. 23, 314–320 (2004).
8. Wiesen, J., Ornstein, M., Tonelli, A. R., Menon, V. & Ashton, R. W. State of the evidence: mechanical ventilation with PEEP in patients with cardiogenic shock. Heart Br. Card. Soc. 99, 1812–1817 (2013).
9. Cross, A. M. Review of the role of non-invasive ventilation in the emergency department. J. Accid. Emerg. Med. 17, 79–85 (2000).
10. Peter, J. V., Moran, J. L., Phillips-Hughes, J., Graham, P. & Bersten, A. D. Effect of non-invasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary oedema: a meta-analysis. Lancet Lond. Engl. 367, 1155–1163 (2006).
11. Sheldon, R. Congestive heart failure and noninvasive positive pressure ventilation. Emerg. Med. Serv. 34, 64–67 (2005).
12. Figueroa, M. S. & Peters, J. I. Congestive heart failure: Diagnosis, pathophysiology, therapy, and implications for respiratory care. Respir. Care 51, 403–412 (2006).
13. Shekerdemian, L. & Bohn, D. Cardiovascular effects of mechanical ventilation. Arch. Dis. Child. 80, 475–480 (1999).
14. Vital, F. M. R., Ladeira, M. T. & Atallah, A. N. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary oedema. Cochrane Database Syst. Rev. CD005351 (2013). doi:10.1002/14651858.CD005351.pub3
15. Mehta, S. et al. Randomized, prospective trial of bilevel versus continuous positive airway pressure in acute pulmonary edema. Crit. Care Med. 25, 620–628 (1997).
16. Nava, S. et al. Noninvasive ventilation in cardiogenic pulmonary edema: a multicenter randomized trial. Am. J. Respir. Crit. Care Med. 168, 1432–1437 (2003).
17. Gray, A. J. et al. A multicentre randomised controlled trial of the use of continuous positive airway pressure and non-invasive positive pressure ventilation in the early treatment of patients presenting to the emergency department with severe acute cardiogenic pulmonary oedema: the 3CPO trial. Health Technol. Assess. Winch. Engl. 13, 1–106 (2009).
18. Park, M. et al. Oxygen therapy, continuous positive airway pressure, or noninvasive bilevel positive pressure ventilation in the treatment of acute cardiogenic pulmonary edema. Arq. Bras. Cardiol. 76, 221–230 (2001).
19. Crane, S. D., Elliott, M. W., Gilligan, P., Richards, K. & Gray, A. J. Randomised controlled comparison of continuous positive airways pressure, bilevel non-invasive ventilation, and standard treatment in emergency department patients with acute cardiogenic pulmonary oedema. Emerg. Med. J. EMJ 21, 155–161 (2004).
20. Levitt, M. A. A prospective, randomized trial of BiPAP in severe acute congestive heart failure. J. Emerg. Med. 21, 363–369 (2001).
21. Pang, D., Keenan, S. P., Cook, D. J. & Sibbald, W. J. The effect of positive pressure airway support on mortality and the need for intubation in cardiogenic pulmonary edema: a systematic review. Chest 114, 1185–1192 (1998).
22. Ram, F. S. F., Wellington, S., Rowe, B. & Wedzicha, J. A. Non-invasive positive pressure ventilation for treatment of respiratory failure due to severe acute exacerbations of asthma. Cochrane Database Syst. Rev. CD004360 (2005). doi:10.1002/14651858.CD004360.pub3
23. Landry, A., Foran, M. & Koyfman, A. Does Noninvasive Positive-Pressure Ventilation Improve Outcomes in Severe Asthma Exacerbations? Ann. Emerg. Med. 62, 594–596
24. Honrubia, T. et al. Noninvasive vs conventional mechanical ventilation in acute respiratory failure : A multicenter, randomized controlled trial. Chest 128, 3916–3924 (2005).
25. Frat, J.P. et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N. Engl. J. Med. 372, 2185–2196 (2015).
26. Patel, B. K., Wolfe, K. S., Pohlman, A. S., Hall, J. B. & Kress, J. P. Effect of Noninvasive Ventilation Delivered by Helmet vs Face Mask on the Rate of Endotracheal Intubation in Patients With Acute Respiratory Distress Syndrome: A Randomized Clinical Trial. JAMA 315, 2435–2441 (2016).
27. Chiumello, D., Coppola, S., Froio, S., Gregoretti, C. & Consonni, D. Noninvasive ventilation in chest trauma: systematic review and meta-analysis. Intensive Care Med. 39, 1171–1180 (2013).
28. Hill, N. S., Brennan, J., Garpestad, E. & Nava, S. Noninvasive ventilation in acute respiratory failure. Crit. Care Med. 35, 2402–2407 (2007).
29. Mas, A. & Masip, J. Noninvasive ventilation in acute respiratory failure. Int. J. Chron. Obstruct. Pulmon. Dis. 9, 837–852 (2014).
30. Mosier, J. M. et al. The Physiologically Difficult Airway. West. J. Emerg. Med. 16, 1109–1117 (2015).
31. Weingart, S. D. & Levitan, R. M. Preoxygenation and prevention of desaturation during emergency airway management. Ann. Emerg. Med. 59, 165–175.e1 (2012).
32. Baillard, C. et al. Noninvasive ventilation improves preoxygenation before intubation of hypoxic patients. Am. J. Respir. Crit. Care Med. 174, 171–177 (2006).
The post Bi-level Ventilation: Who Needs it and Who Doesn’t? Pearls and Pitfalls appeared first on emdocs.
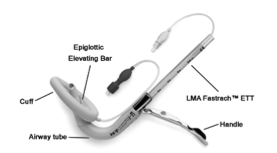

































 This blog post is the second part of a series of 3, on a recent lecture I was asked to give on Critical Care Updates: Resuscitation Sequence Intubation. This talk was mostly derived from a podcast by Scott Weingart (Twitter: @EMCrit) where he talked about the
This blog post is the second part of a series of 3, on a recent lecture I was asked to give on Critical Care Updates: Resuscitation Sequence Intubation. This talk was mostly derived from a podcast by Scott Weingart (Twitter: @EMCrit) where he talked about the